What happens next?
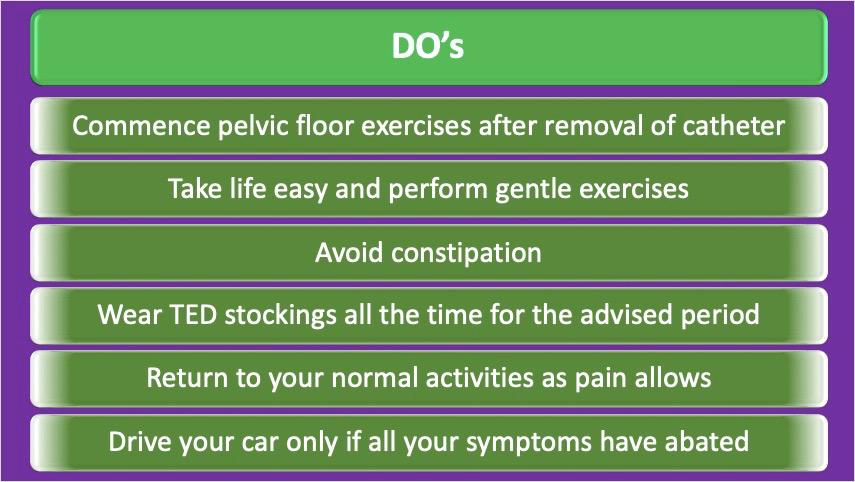
It is standard practice to carry out RP 4-6 weeks after transrectal biopsies. It is very useful to spend this time learning (from a physiotherapist) and performing pelvic floor exercises regularly – this will help regain continence earlierin the post-op period.
RP is considered as a major pelvic operation. Therefore, you are likely to undergo assessment to check your heart and lung functions, in addition to the standard blood tests and x-rays / scans. An anesthetist will see you after this.
Although with laparoscopic and robotic RP the blood loss is quite minimal we tend to reserve 2 units of blood in the unlikely event of you requiring a blood transfusion either during or after the operation.
What happens after I get admitted to hospital?
You are likely to be admitted the evening before surgery. You are likely to get an enema that evening and another one the following morning prior to surgery. You will be fasting from midnight (if surgery is scheduled for the morning) and may get an intravenous ‘drip’ to keep you well hydrated.
You will be fitted for some special stockings (thrombo-embolic deterrent – TED).
These prevent you from developing clots(deep vein thrombosis – DVT) in your legs. You will need to wear these before being taken to the operating rooms. You will also receive injections of heparin following the operation to protect against DVT. I generally advise my patients to wear TED stockings for a period of 4 – 6 weeks after RP.
What happens after the operation?
You will be shifted back to the ward normally, but in case of longer operating time may be shifted to ICU for post-op care. You will be able to drink fluids a few hours after the operation and resume normal diet within 12-24 hours.
If you have had an open operation the longer / larger wound may require strong painkillers or even a PCA drip (Patient Controlled Analgesia) that allows smooth and uninterrupted pain relief. If you have had a robotic RP, the need for painkillers is not as prolonged.
You will have an intravenous drip running for several hours. This will be stopped after 12 hours or so. There will be a drain tube coming through the lower part of your abdomen. This is usually removed in 24 hours. A urinary catheter will drain your bladder. The urobag that collects urine draining through your catheter will be changed to a ‘leg bag’ (this is attached to your leg) when you leave hospital. This allows you to walk freely without having to carry the urine bag in your hand.
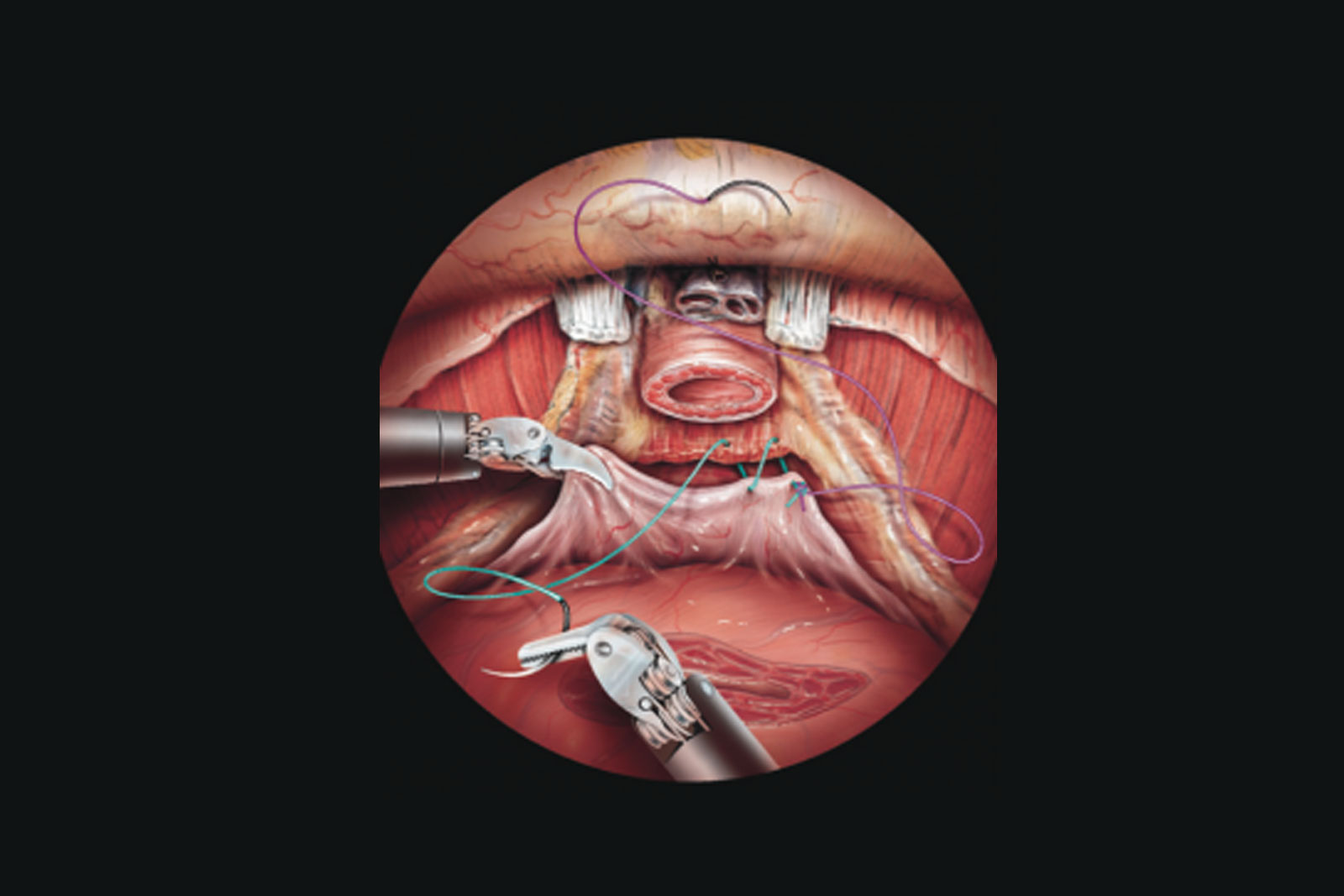
It is important to remember that the catheter is ‘protecting’ a very delicate ‘join’ (anastomosis) between the bladder and the urethra. Therefore, it is of utmost importance that any problems with the catheter (getting dislodged, pulled, cut, etc.) are reported immediately. If such a problem occurs after you have been discharged home please report to the hospital immediately.
When anybody has a catheter it is common to get ‘bladder spasms’ – this is basically your bladder trying to get rid of a foreign body i.e. the catheter. This manifests with either pain in the bladder area (lower part of the abdomen) associated with a desire or urge to pass urine or actual leakage of urine around the catheter. If this becomes problematic, medication can be given to deal with the symptoms.
When will the catheter be removed? Will I have any difficulty passing urine after this?
The catheter is usually left in place for 10-14 days. You would have a date arranged for removal of catheter before you leave hospital.Once the catheter has been removed urine is passed normally through the penis.
In addition some patients find they do not get a lot of warning about the need to pass urine and it may be quite frequent. This is due to continued healing of the sensitive part of the bladder.
The pelvic floor exercises will assist in this recovery process. It is useful to have a supply of sanitary pads to manage any leakage.
I generally see my patients when they come for removal of catheter. This is also a good time to discuss the results of the histopathology examination (HPE) of the prostate.