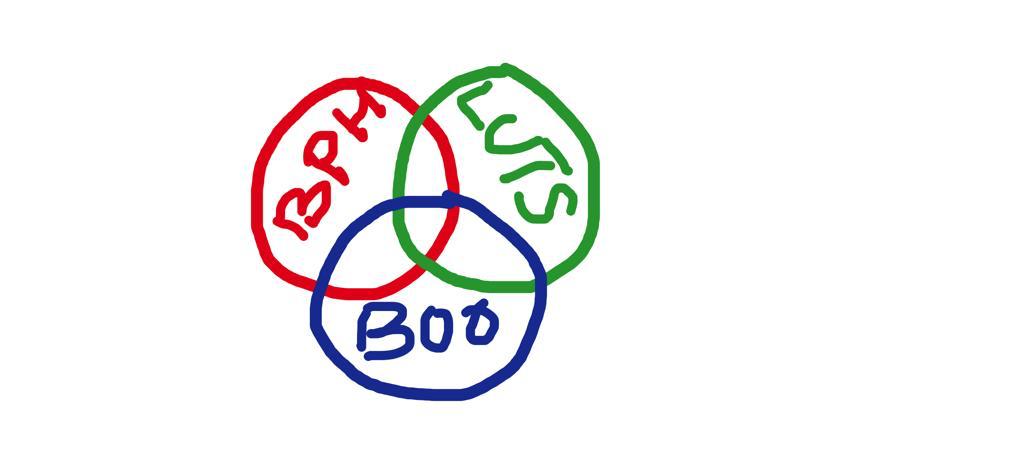
Storage symptoms refer to difficulty with storing urine in the bladder. These symptoms can be caused by a variety of causes both benign and malignant. Storage symptoms include:
Frequency
Nocturia (frequent urination at night)
Urgency (feeling of a sudden need to urinate)
Urge incontinence (involuntary loss of urine related to urgency)
Stress incontinence (involuntary loss of urine related to straining eg. lifting a heavy object or sneezing or coughing)
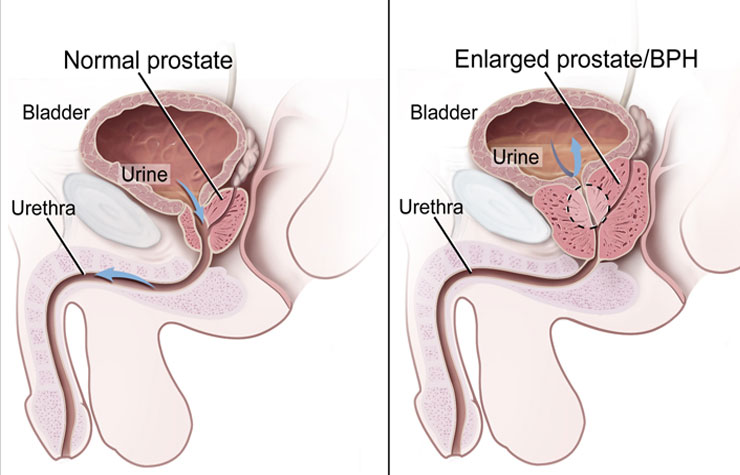
HOW IS BPH / LUTS MANAGED BY THE UROLOGIST?
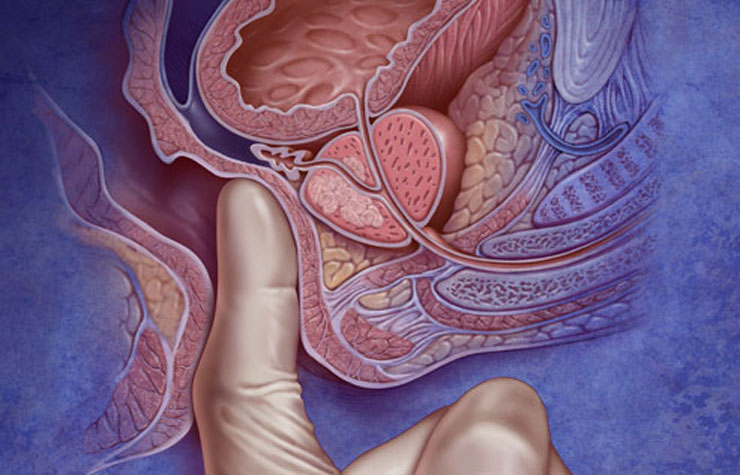
After taking your medical history, the urologist will perform a clinical examination including a digital rectal examination (DRE) to evaluate your prostate.
You may be asked to fill out a chart of the number of times you pass urine and / or the amounts passed each time (frequency / volume chart).
Following this he/she may order some tests, which may include some or all of the following:
Urine analysis and bacterial culture tests (the urologist might refer to this as an MSU for m/c/s – mid-stream urine for microscopy/culture/sensitivity)
Uroflow test – to assess your urinary flow – you will be asked to void into a machine which records the flow of urine against time (flow rate)
Bladder scan to assess your bladder emptying (post-void residue – PVR)
PSA (Prostate Specific Antigen – see PSA – pt guide)
Creatinine and electrolytes (this is to evaluate your kidney function)
Ultrasound scan of your kidneys and bladder (USS-KUB)
Flexible cystoscopy (see CYSTOSCOPY – pt guide)
Transrectal ultrasound guided biopsies of the prostate in case your PSA is elevated (see TRUS-PROSTATIC BIOPSIES – pt guide)
Urodynamics – this is a functional study of the bladder
Following review of the test results, you are likely to be recommended one or more of the following:
Lifestyle modification eg. restricting fluids / avoiding caffeinated drinks
Pelvic floor exercises
Medications
Surgery (see TURP – pt guide)
If PSA is elevated and biopsies confirm prostate cancer (see PROSTATE CANCER – pt guide) your urologist will discuss about management options for this.