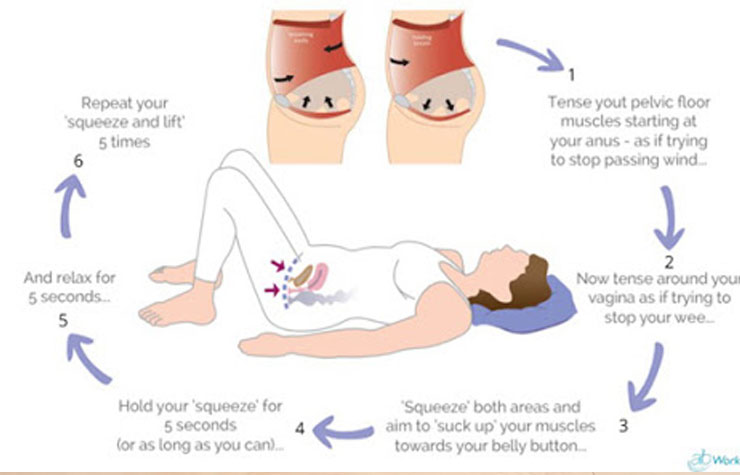
1. Sit in a chair with your knees slightly apart. Imagine you are trying to stop wind escaping from your anus (back passage). You will have to squeeze the muscle just above the entrance to the anus.
You should feel some movement in the muscle. Don’t move your buttocks or legs.
2. Now imagine you are passing urine and are trying to stop the stream. You will find yourself using slightly different parts of the pelvic floor muscles to the first exercise (ones nearer the front). These are the ones to strengthen.
If you are not sure that you are exercising the right muscles, put a couple of fingers into your vagina. You should feel a gentle squeeze when doing the exercise.
1. You need to do the exercises every day.
2. Sit, stand or lie with your knees slightly apart. Slowly tighten your pelvic floor muscles under the bladder as hard as you can. Hold to the count of five, and then relax. Repeat at least five times. These are called slow pull-ups.
3. Then do the same exercise quickly for a second or two. Repeat at least five times. These are called fast pull-ups.
4. Keep repeating the five slow pull-ups and the five fast pull-ups for five minutes.
5. Aim to do the above exercises for about five minutes at least three times a day, and preferably 6-10 times a day.
6. Ideally, do each five-minute bout of exercise in different positions. That is, sometimes when sitting, sometimes when standing, and sometimes when lying down.
7. As the muscles become stronger, increase the length of time you hold each slow pull-up. You are doing well if you can hold each slow pull-up for a count of 10
8. Do not squeeze other muscles at the same time as you squeeze your pelvic floor muscles. For example, do not use any muscles in your back, thighs, or buttocks.
9. In addition to the times you set aside to do the exercises, try to get into the habit of doing exercises whilst going about everyday life. For example, when answering the phone, when washing up, etc.
10. After several weeks the muscles will start to feel stronger. You may find that you can squeeze the pelvic floor muscles for much longer without the muscles feeling tired.
It takes time, effort and practice to become good at these exercises. It is advised that you do these exercises for at least three months to start with. You should start to see benefits after a few weeks. However, it often takes 8-20 weeks for most improvement to occur. If possible, continue exercising as a part of everyday life for the rest of your life to stop the problem recurring.
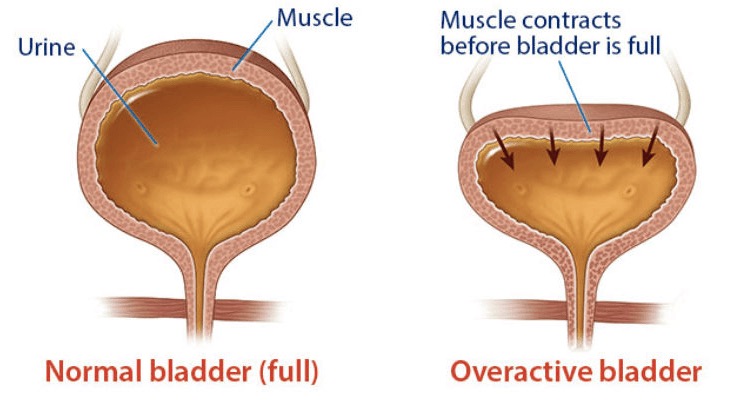
Medication: You may be prescribed some tablets (in the family of anti-muscarinics) to slow down the frequency and strength of unwanted bladder contractions. These tablets have some side effects and the urologist will discuss these with you.
BoTox: Injection of botulinum toxin into the bladder wall is an alternative once the trial of medications is exhausted and symptoms persist. This is a relatively expensive affair and the urologist will discuss this with you.
Surgery: A few options are available in the worst affected cases. Again, the urologist will discuss these with you.