What is ureteroscopic laser treatment of stone?
It is most likely that a stone has dropped from the kidney into the ureter. Your doctor may have then determined, based on your particular clinical circumstances, to treat your stone by ureteroscopic laser fragmentation. You may or may not have had a ureteric stent put in prior to this.
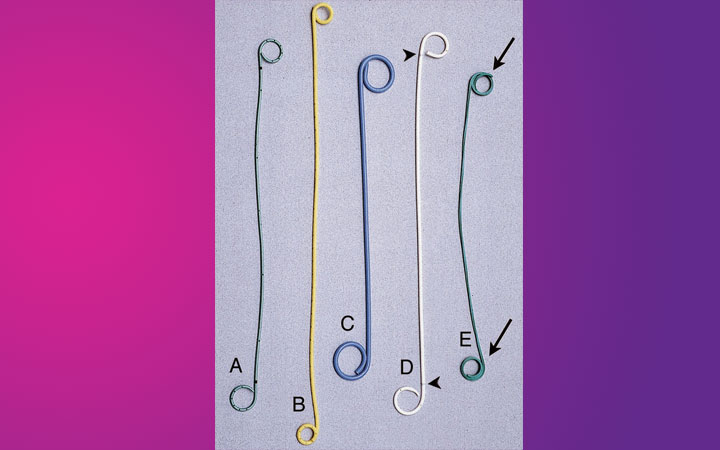
Ureteroscopy is done under GA, the stone is reached and is then broken up by using the Holmium:YAG laser (see URETEROSCOPIC LASER FRAGMENTATION OF STONE – video). If there are large fragments, these are likely to be removed using a basket (pic on left). This allows chemical analysis of the stone as well. If the stone has been broken to fine dust these will pass out naturally – likely to be noticed as ‘sand’ in your urine.
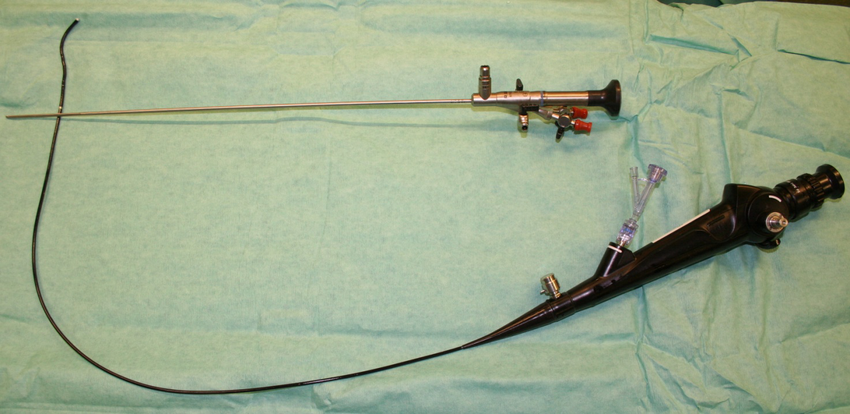
What is different about flexible ureteroscopy?
Whilst a rigid ureteroscope is used to manage problems in the ureter, a flexible ureteroscope is used to manage problems in the kidney. Flexible ureteroscopy is a highly specialized procedure and is best undertaken by experts in this field.
Will I have a stent inserted after the ureteroscopy?
This will depend on the individual circumstances, but the urologist will make this decision after he has done the ureteroscopy, whether it has been done for diagnostic or treatment purposes.
Will I be able to go home after ureteroscopy?
Most diagnostic ureteroscopy patients will be going home the same day. In the case of patients with stones, the majority tends to be done as a day case (this depends on the time the procedure is done during the day). Also, you may have an x-ray taken after the procedure to check stone clearance as well as stent position.
Do I need to take any precautions or avoid doing anything after ureteroscopy?
Your doctor will advise you about fluid intake, which usually needs to be plenty. Most will be able to resume normal activities within 24-48 hours. There are no specific restrictions apart from those related to having had a general anaesthetic (for example: do not drive or operate machinery for 24-48 hours).
What is PCNL?
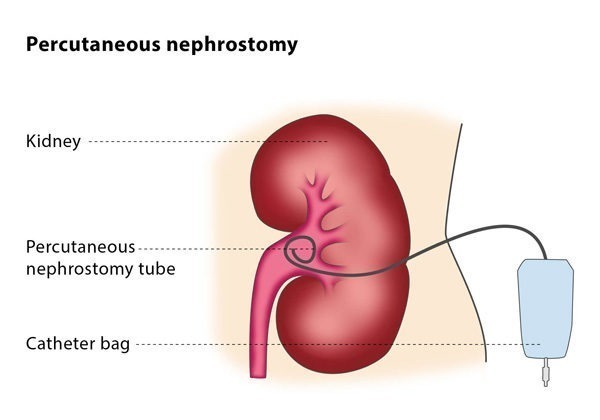
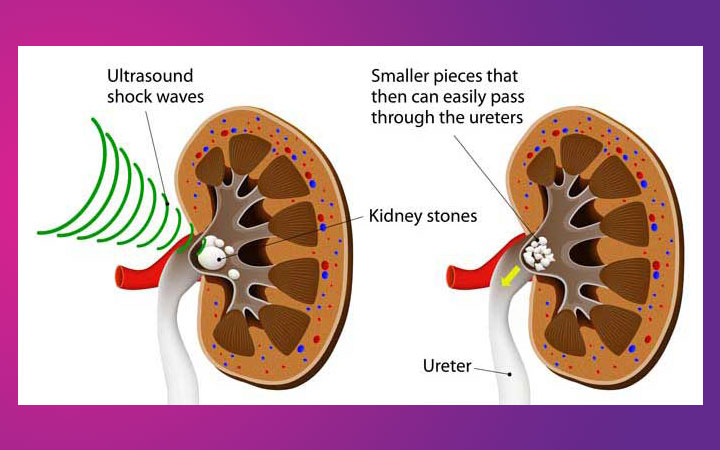
This is a surgical procedure where stones from the kidney are removed directly by making a puncture into the kidney through the skin; the stones are broken into fragments either by a lithoclast or using laser energy.
The fragments are then removed, following which a tube (nephrostomy tube) is left in the kidney for 24-72 hours.
Does this require general anaesthesia (GA)?
Yes, this is commonly done under GA.
What happens after the procedure is done?
You can expect to have a nephrostomy tube coming from the side of your tummy, a urinary catheter draining your bladder and a drip for intravenous fluids, when you are brought out of the operating room. You can expect to resume normal diet within a few hours.
You will usually have an x-ray taken to check clearance of stone fragments the following day, in addition to routine blood tests.