If you have these symptoms, it is likely that you have benign enlargement of your prostate, but it is best to check with your urologist to rule out the presence of clinical prostate cancer.
In advanced or metastatic prostate cancer, it has a tendency to spread to bones, commonly the spine, pelvis, thigh bone and ribs. Pain in these regions can be the presenting symptom in some men.
In locally advanced prostate cancer, the ureters (the tubes that bring the urine from the kidneys to the bladder) can be obstructed by the tumour and cause kidney failure.
Are there any tests to find out if I have prostate cancer?
The diagnosis of prostate cancer is based on the following:
Digital rectal examination (DRE): this involves the urologist inserting a gloved finger through your back passage (rectum) and examining your prostate. This is good at detecting nodules or hardness of the prostate and advanced cancer of the prostate. The prostate remains normal in early prostate cancer.
Prostate specific antigen (PSA): please see PSA – pt guide
Transrectal ultrasound guided prostatic biospies (TRUSPBx): see TRUS-PROSTATE BIOPSY – pt guide
In men who have an elevated PSA and negative prostatic biopsies, but with persisting suspicion of underlying prostate cancer, the urologist may recommend further testing. This requires a highly individualized approach and is best discussed with the urologist.
Sometimes prostate cancer is diagnosed incidentally following transurethral resection of prostate (TURP) – a surgical procedure to treat symptomatic benign enlargement of the prostate. Your urologist will discuss further management of this.
What happens if prostate cancer is diagnosed in my case?
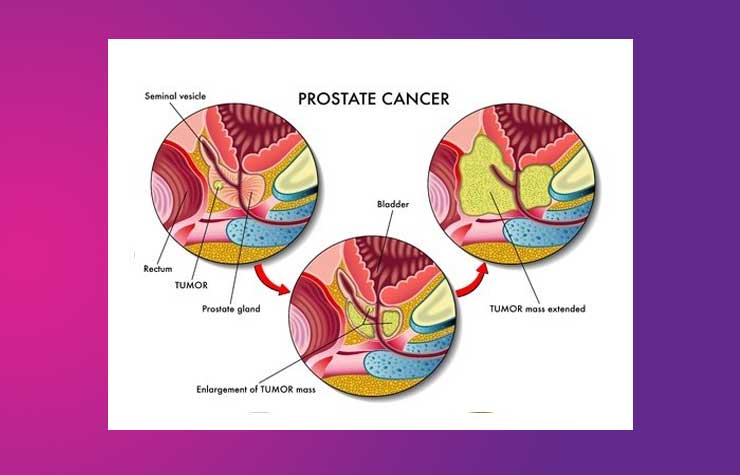
There are three distinct clinical entities with regards to prostate cancer:
Early prostate cancer (EPC): where diagnosis is made by needle biopsy. Not everybody with EPC may need treatment. Treatment options will depend on the level of PSA, the volume of cancer detected at biopsy and the grade of the cancer. Most men with EPC will not die from it, especially if you are in your 70s or 80s.
You are likely to be recommended either surgery or radiotherapy as radical treatment options (ie intent to cure). If you are elderly or have other significant medical problems, your urologist may recommend mere watchful waiting with a view to initiating treatment at the onset of symptoms. Before these decisions are made your urologist may recommend further investigations including MRI or CT scan of your pelvis and a bone scan.
Locally advanced prostate cancer (LAPC): Here the tumour has enlarged to a significant extent and may be getting into nearby tissues like bladder, ureters, rectum or pelvic bone. This indicates its aggressive nature and will require treatment – you are likely to be recommended radiotherapy (RT) along with hormonal therapy (HT) or just HT alone.
Metastatic prostate cancer (MetPC): Here the cancer has spread to other parts of the body, commonly lymph nodes and bones, but occasionally to other organs. The intent in this situation is to treat symptoms ie palliation. HT is the mainstay of treatment. In some patients, HT may be delayed until onset of symptoms. Bone pain may require radiotherapy to the part that is affected.
What are the curative options if I have early prostate cancer (EPC)?
Broadly speaking this involves either radical surgery or radiotherapy.
Radical prostatectomy (RP): This involves removal of the whole prostate. See PROSTATE SURGERY – pt guide.
Radical radiotherapy (RT): External beam radiotherapy (EBRT) as it is called, involves treating the prostate with high-energy rays. This is usually combined with HT for 3 – 6 months.
Both RP and RT can cause urine leakage and problems with erection. RT, in addition, can cause bleeding from the rectum and frequent loose motions.
What is hormonal therapy (HT)?
Prostate cancer cells require testosterone for its growth. Hormonal therapy or androgen deprivation therapy (ADT) aims to lower the testosterone level in the body by means of tablets, injections or surgery (removal of the testes). HT doesn’t kill but slows or stops the growth of cancer cells for many years.
Side effects of HT include lack of energy, weight gain, breast swelling, hot flushes, erection problems and lowered sex drive. Anaemia (low haemoglobin) can be a problem as much from the cancer as it is sometimes due to HT.
For a more detailed discussion on prostate cancer please contact your urologist.